Lung Cancer

Diagnostics Tests For Lung Cancer
Clinical History & Examination: The doctor will ask for symptoms such as persistent cough, coughing blood, repeated chest infection, chest or shoulder pain, breathlessness, hoarseness of the voice, weight loss and wheezing. A examination will also be done to examine the chest, lymph nodes in your neck. The doctor may also ask for blood tests such as Complete blood count to measure the number of white blood cells, red blood cells and platelets to get information on the patients overall health. Other tests such as alkaline phosphatase (ALP), calcium or phosphorus, liver function tests are used to gauge whether the cancer has spread to organs such as the liver and bones.
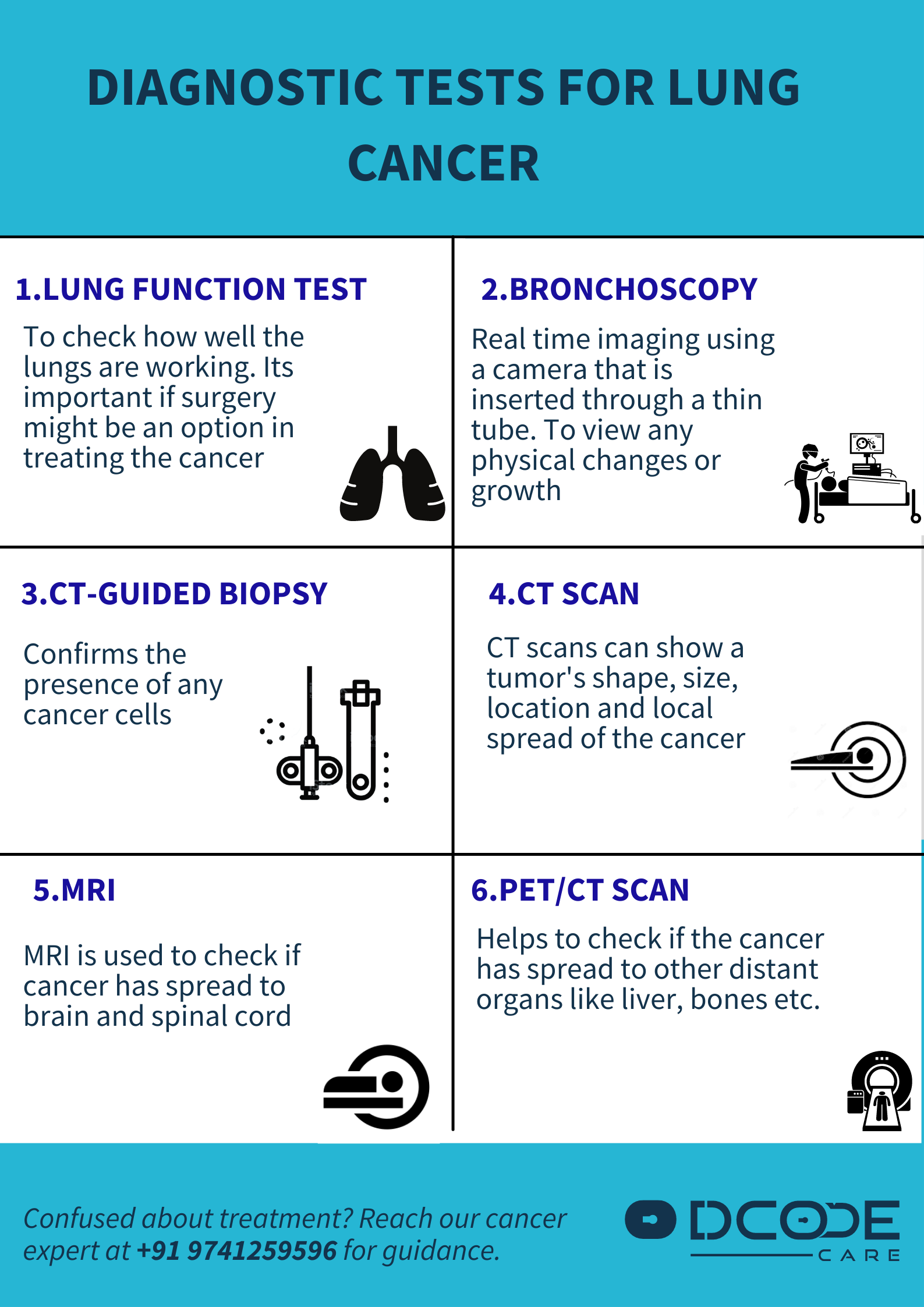
Pulmonary Function Tests: Pulmonary function tests are used to measure how well the lungs are working. There are a number of tests such as spirometry (measures how much air can be breathed in and out of the lungs), plethysmography (measures how much air is taken in to the lungs after a deep breath and how much air is left in the lungs after forcefully breathing out), lung diffusion test (measures how well oxygen moves from the lungs into the bloodstream).
Imaging tests: X-ray - An image of the lungs may reveal abnormalities such as a mass or a nodule. CT scan: A CT scan is useful to detect small lesions in the lungs that may be missed on X-ray. MRI: MRI scans are useful for staging of the cancer. Certain diagnostic tests may be used to detect the spread of the disease to other organs such as positron emission tomography (PET) and bone scans.
Tissue sample or Biopsy: A sample of abnormal cells may be removed in a procedure called a biopsy by procedures such as bronchoscopy (a lighted tube that's passed down the throat and into the lungs) mediastinoscopy (an incision is made at the base of the neck and surgical tools are inserted behind your breastbone to take tissue samples from lymph nodes;) and needle biopsy (X-ray or CT images are used to guide a needle through the chest wall and into the lung tissue). Thoracoscopy is another minimally invasive procedure to examine the outer lining and the surface of the lungs and collect samples in the case a suspicious area is noted. Oesophageal ultrasound-guided sampling (EUS) is a technique used to confirm the spread of cancer to nearby lymph nodes if suggested based on radiological scans.
Cytology: (or cytopathology) is the examination of cancerous cells that spontaneously detach from the tumour. These samples are obtained by Bronchoscopy (Bronchial washings with a mild salt solution in the airways), Thoracentesis/pleural drainage (Pleural effusion is the abnormal collection of fluid between the thin layers that surround the lung. The fluid is collected using a fine needle) and Pericardiocentesis/pericardial (Pericardial effusion is an abnormal collection of fluid between the layers that surround the heart and which is drained using a fine syringe).
Additional Videos
Treatments Of Lung Cancer
- Surgery: The objective of the surgeons is to remove all the cancer in the lung or in advanced cases to remove a part of the tumour that leads to symptoms affecting the quality of life. There are various procedures that may be implemented: Wedge resection (the procedure involves the removal of a small section of lung containing the tumor and a margin of healthy tissue), Segmental resection (removes a larger portion of lung, but not an entire lobe which is a subpart of the lung), Lobectomy (remove the entire lobe of the lung) and Pneumonectomy (removal of an entire lung). In larger tumours it may be recommended to receive chemotherapy or radiation therapy before surgery in order to shrink the tumour. Advancements in lung cancer surgery include minimally invasive surgery and video-assisted thoracoscopic surgery (VATS), which reduce the amount of time spent in the hospital post-surgery but are indicated only in specific conditions. Side effects: Pain, air leak, pneumonia, infection.
- Radiotherapy: Radiation therapy uses high-powered energy beams to kill cancer cells. In patients with advanced lung cancer restricted to the lungs, radiation may be used before surgery or after surgery and is often combined with chemotherapy treatments. If patients in whom surgery isn't an option, combined chemotherapy and radiation therapy may be the primary choice of treatment. Side effects: Skin damage, blisters, difficulty swallowing, heartburn or indigestion, radiation pneumonitis (an inflammation leading to cough, fever and fullness of chest).
Stereotactic body radiotherapy: It is also known as radiosurgery. It is an intense radiation treatment that aims beams of radiation at the cancer. It may be an option for patients with small lung cancers who can't undergo surgery and in patients in whom the cancer has spread to other parts of the body.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells and is given through a vein or taken orally. A combination of drugs usually is given in a series of treatments over a period of weeks or months. It is often used before surgery to shrink the tumour or after surgery to kill any cancer cells that may remain. It can be used alone or combined with radiation therapy. Side effects: Depending on the agent used these may differ but common side effects include anemia, fatigue, nausea, lowered immunity, anorexia, nerve damage, increased risk of bleeding, loss of hair, mouth ulcers, swelling of legs, nausea, vomiting, muscle pain etc.
- Targeted drug treatments: These agents block specific chemicals and pathways present within cancer cells, causing them to die. These agents are most commonly reserved for people with advanced or recurrent cancer. Side effects: Depending on the agent used these may differ but common side effects include: decreased appetite, diarrhoea, nose bleeds, nausea, rash, acne, dry skin, itchiness, vomiting, constipation, muscle and joint pain, swelling of legs, hypertension , lowered immunity, anorexia, nerve damage, increased risk of bleeding etc.
- Immunotherapy: Immunotherapy uses the body’s immune system to fight cancer. Immunotherapy interferes with the process of blocking the immune system that is used by some cancer cells. Patients whose tumours express high levels of a specific PD-L1 protein based on molecular testing using a tumour biopsy may receive first-line immunotherapy with a specific agent called pembrolizumab. Side effects: Depending on the agent used, these may differ but common side effects include: Back pain, cough, decreased appetite, diarrhoea, rash, difficulty in breathing etc.
- Photodynamic therapy: Photodynamic therapy is also called PDT and is a form of treatment that kills cancer cells by using a combination of a light sensitising drug followed by a very bright light. It is used in patients in whom the cancer is too advanced or the patient is not healthy enough to undergo aggressive therapy. PDT can shrink the tumour and relieve symptoms in these patients.
- Side effects: Light sensitivity, skin rashes, blisters, body soreness etc.
- Palliative care: People with lung cancer experience symptoms of the cancer, as well as side effects of the various types of treatment. Palliative care specialists work to minimize these symptoms and improve the patient’s quality of life as well as reduce the anxiety and depression involved with the cancer diagnosis.
Sources: American Cancer Society; European Society for Medical Oncology (ESMO); Canadian Cancer Society; Mayo Clinic;Cancer Research UK;